Whine Flu
By now, you’ve probably heard something on the news about a new strain of influenza that’s going around. There’s been just a bit of coverage about it.
While listening to the online and face-to-face chatter, it seemed like most reactions fit neatly into two categories:
1. Fear/caution/preparedness/”The sky is falling”. Symptoms include altering trips or school in absence of personal illness or the advice of public health officials; stockpiling large amounts of food, antiviral medicines, face masks, or other supplies; foregoing pork; and flat-out panic upon hearing someone cough.
2. Indifference/outrage/ridicule of those in Group 1. Symptoms include derisive responses to public health warnings; argument that “the media is making this up” and “thousands of people die of the flu every year and only a handful have even gotten sick with this strain, so it’s all nonsense”. This occasionally advances to government conspiracy theories.
I have the upmost respect for both types of responses, each of which has some kernel of rational thought. Furthermore, many people will shift between one mindset and the other. That being said….
Those in Group 1 are wrong. They’re also right.
Those in Group 2 are right. They’re also wrong.
To understand why this is not just Alice-in-Wonderland doublespeak, let’s consider seasonal influenza in comparison to pandemic influenza. And to do that, it’s worth marveling at the biology of viruses.
Different viruses cause a range of diseases: the common cold, HIV/AIDS, smallpox, polio, influenza – just to name a few. Viral particles, or virions, are at the edge of living and non-living. Mere bits of nucleic acid encoding a very few genes and coated in protein, they don’t even have cells. (They don’t need to; they just hijack them.) They can lay dormant for minutes, hours, or years; in some cases withstand extreme heat or cold; and – rarely, but sometimes to devastating effect – can jump from one host species to another. When they infect a host, if they are successful, they have but one objective: to take over the host’s own cells to make more copies of themselves. If such a scrap of non-life could be said to have an ego, they would be narcissistic to the extreme – constantly muttering, “me, and more of me, and more of me…”
The most virulent types of viruses will do this without regard for the survival of the original host. This might seem short-sighted, until you consider that if their progeny can infect other individuals who come in contact with the first host, then it’s not such a dead end after all. All they have to do is make more of themselves; it matters not in whose body this occurs.
Battles between viruses and hosts occur throughout the biological world. It’s one of the cards living organisms are dealt, and when all goes well, we are unaware of the constant viral bombardment our bodies experience. Human immune systems deftly respond to the viruses we come into contact with, sizing up the danger, dispatching them before they cause trouble.
Until that system fails, and we get sick. Who hasn’t had a case of seasonal influenza? Every year, up to 20% of the U.S. population comes down with it – one in five people! – so it is extremely rare to go through your life and never have experienced the symptoms of fever, sharp headache, fatigue, muscle aches, cough, congestion, and sometimes stomach ailments. The telltale sign: you realize you feel slightly off, and then it’s like you’ve been hit by a truck that parks itself on your chest for at least a week, maybe two. That’s the difference between REAL influenza and all the other minor ailments we refer to as “flu”.
Now, the key thing to understand is that viruses are populations that evolve and change and mutate and recombine over time. It’s not one “virus”. It’s a seething, morphing, moving mass of viral particles that evolves with fury. So the strains of influenza virus that are most dominant in one year are almost never the same strains that will cause trouble the next year.
This is why the seasonal flu vaccine has to be prepared anew each season. Influenza experts in the U.S. do their level best, every year, to predict the future. They assess all the data at hand on what strains of influenza are circulating in the environment and the human population months before the upcoming season.
Then they make a guess as to which strains will win out come fall.
Then they ask the manufacturers of influenza vaccines to please make several million doses of vaccine to cover that year’s predicted cocktail.
Then they wait, and hope that they didn’t screw up.
In a normal year, about 36,000 people in the U.S. will die of seasonal influenza anyway. Maybe less – if the strains going around aren’t terribly virulent, and the flu experts guessed right about the vaccine. Maybe more – if they strains are strong, and the flu vaccine missed the mark, or not enough of the population is immunized*.
But the thing to realize is that the vast majority of people who die from seasonal influenza fall into at least one of three categories: the very old, the very young, and the already-ill. Often it isn’t the influenza that actually causes their demise; it’s a secondary infection such as pneumonia that their inadequate immune systems just can’t overcome.
But every so many years something different happens. A new strain, a new kid on the block, starts going around. It’s different from the others. It likely just recently discovered how hospitable humans could be as a host. Before it started looking at us as prime real estate, it preferred to cause misery in another host species. Birds, say. Or pigs. It helps if it’s a species in which there is a reasonable amount of human-animal contact, because it first makes the jump from the animal to the human caretaker.
Sometimes this ends up being a dead end for the influenza strain. It can jump from pigs to humans as a one-time deal, but can’t transmit farther.
And then sometimes, it accumulates another mutation or two, swaps another gene with a different influenza virus strain, and voila – it’s new and improved. Stronger. Better. It’s capable of human-to-human transmission.
In other words, it’s a potential pandemic strain.
So what do you look for in a pandemic influenza strain? Well, ideally it has a high rate of person-to-person infectivity. It will be completely unknown to the global human population, so it trips up immune systems that have never encountered it before. It will thus have a different pattern of infection: it will hit relatively young adults very hard. Now remember, young adults may get seasonal influenza, but they don’t normally die of it unless they have underlying health problems. With a pandemic strain, though, all bets are off.
So, how bad can pandemic influenza outbreaks get? Well, it depends on the strain and the times. Let’s look at the 1918 global influenza pandemic outbreak, for example. It’s a classic.
In the spring of 1918, there was a global wave of illness that was noticeable, but mild in terms of deaths. Autumn, however, brought the first of two more waves that were absolutely lethal. It’s been estimated that a total of 500 million people - or one-third of the world’s population at the time - fell ill by the time the epidemic was over. Of this, between 50 million and 100 million people worldwide died. The case fatality rates were over 2.5%, as compared to about 0.1% for typical seasonal influenza.
Put in perspective – if the same pandemic were to occur today given an estimated global population of 6.77 billion, 2.25 billion people worldwide would fall ill, and over 56.4 million people would die by the time the epidemic was over.
The thing is, when the 1918-1919 influenza outbreak happened, public health officials didn’t even know it was influenza. It happened too fast, spread too quickly, killed too quickly. In some cases it actually killed within hours, not days. We now know this was due to a violent overreaction by the immune system to the novel strain, causing viral pneumonia and what is termed a “cytokine storm”. The result? Massive, rapid filling of the lungs with fluid.
At the time, medical experts thought the disease was caused by a bacterium, not a virus. The pathogenic agent wasn’t identified until the 1930s. And it wasn’t until the mid-1990s that the genetic sequence was painstakingly reconstructed by researchers at the CDC using preserved autopsy specimens so scientists could try to figure out what was so very different about this strain.
Now keep in mind that there were a lot of other factors at play in 1918-1919. Lifesaving tools like respirators, antiviral medications, and antibiotics to treat secondary infections were either in limited supply or nonexistent because they hadn’t been developed yet. And World War I played a role; fighting was heavy throughout the spring and summer; troops were being shipped to and fro; and millions of people in Europe were displaced, on battlefields, taken prisoner, and otherwise subject to poor sanitation and health. Armistice didn’t occur until November 11, 1918, and the aftermath of war in terms of public health continued for months to years.
Mysteries remain, though we now know more about the strain itself. Virologists classify influenza strains in terms of the “flavor” of two particular proteins that are found on the viral coat: hemagglutinin, or “H”, and neuraminidasae, or “N”. The strain that caused the 1918 epidemic was an influenza A(H1N1) strain. Its origin is still unknown. Genetically, it appears to have started off infecting pigs, but the actual location from which it originated is still unknown. There is no smoking gun, or hog, as it were.
OK, so fast-forward to April 2009. One of the jobs of public health officials all over the world is to keep tabs on disease outbreaks of any kind, and the World Health Organization is charged with coordinating communication and response.
So medical practitioners in Mexico started to notice something. There was a large spike in influenza cases. This is atypical for the warmer months of spring and summer. Influenza virions usually survive and transmit more easily in cold, dry weather, when they hang in the air longer and people are congregated indoors. Even more alarming, it was causing what appeared to be an abnormally high death rate. And further? The people who were dying were young adults – in their 20s and 30s. Preliminary testing indicated it was a strain of influenza A, and appeared to be related to a strain of influenza that is endemic in pigs, but beyond that it couldn’t be typed.
So let’s think back again to the hallmarks of a pandemic influenza strain: novel? Check. Person-to-person transmission? Check. Kills young adults? Check.
You can now see why public health officials all over the world started to sweat.
The response over the next ten days was swift, and from all accounts thus far, effective. Mexico took measures to control the outbreak that included shutting down schools and public gathering places for a period of time. The Centers for Disease Control developed assays to determine the strain and began scaling up test processing. Healthcare officials set guidelines for patient testing and within days the pattern of disease became much clearer. Laboratories with expertise in growing “seed strains” for vaccine development were pressed into service. Clinical diagnostic technicians worked round the clock to process test samples. And by April 27, scientists at the CDC had completed sequencing the genome of the new strain and made the data available for researchers all over the world to examine.
As time progressed, public health officials began to be cautiously optimistic. It looked like the number of cases and deaths were lower in Mexico than initially projected, and although the disease was spreading, the death rate outside of Mexico appeared very low for reasons that are still not completely understood. Analysis of the strain’s genome indicated that while the 1918 pandemic strain was an ancestor, it lacked some of the features of the 1918 strain thought necessary for high lethality.
However, caution is still warranted. Though the number of hospitalizations in the US have remained low, the average age of patients hospitalized with this strain is only 15. The months to come will bring careful monitoring by the WHO and CDC. After all, this strain could easily evolve into a more virulent form. The very worst thing we could do is collectively ignore the advice of public health officials in coming months.
So was the response overblown? In a word, no. That’s the irony of addressing pandemic disease threats: when the response goes as it should, nothing happens. Beautiful, beautiful nothing. Public health experts are always in a difficult bind. If they sound a global alarm, their recommendations can bring travel, trade and economic growth to a screeching halt. And depending on the risk level of a particular outbreak, it is arguably worth it. But second-guessing after the fact is largely fruitless. If disease breaks out in spite of control measures, then we didn’t do enough. If it doesn’t break out, either we did enough, or it wasn’t going to happen anyway. But as you can appreciate, the risk in this case was very, very real – and the response has been dialed back appropriately as new information came in.
For comparison, let’s keep the impact of this in context with other viral diseases. Below I’ve charted average yearly deaths due to AIDS, rabies, ebola, seasonal influenza, and the pandemic influenza of 1918 – all diseases caused by viruses. The viruses with the highest lethality rates are actually rabies, which is 100% lethal if untreated, and ebola, which can be up to 90% fatal. But each of these viruses has fairly limited transmission patterns. Rabies in industrialized nations has been kept in check by vaccination programs for companion animals and sometimes even for at-risk wildlife. Ebola, like other hemorrhagic fevers, is highly lethal and contagious – but since it is transmitted from animals in remote rainforest areas of African nations, outbreaks thus far have been limited to small villages that have little interaction with major population centers. Seasonal influenza results in between 250,000-500,000 deaths annually. AIDS-related deaths top 3.1 million, and AIDS is a much, much more serious threat in the long term because these deaths occur year after year after year; whole generations are being lost, particularly in African nations. However, you can see that as far as death toll within a single epidemic year is concerned, a severe pandemic influenza outbreak tops them all. This is because influenza in general is more easily transmitted. Unlike HIV or rabies, it can be spread by coughing, sneezing, or touching surfaces that have respiratory secretions on them.
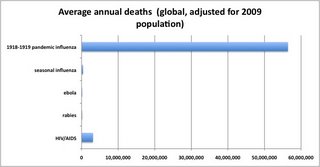 (click on image to enlarge)
(click on image to enlarge)The moral of the story? Listen carefully to the official CDC and WHO guidelines, and realize that recommendations are made soberly and deliberately by some of the best public health experts in the world. Take low-cost but effective measures like washing your hands and your childrens’ hands, and if you or your family members become sick, take the time needed to recovery fully before heading back to work or school. Don’t live in fear. We are fortunate to be living in a time when science and medicine both allow information to be shared quickly and treatments to be widely available. Don’t stockpile antiviral drugs – save them for people who really need it. If you were to fall ill, you’d get the meds you need. In a pandemic, they are distributed on the basis of need, even to those lacking health insurance. And be a critical consumer of the most sensational news coverage; challenge journalists who you think might be presenting dubious information.
Finally, realize that if the situation changes, often it’s because the virus itself has evolved. It could fizzle out within the population, or it could pick up a few changes here and there and become more fierce.
Note: The title “Whine Flu” came from a very non-scientific Facebook survey in which I solicited from friends some new-and-improved names for influenza A(H1N1). The name “whine flu” was submitted by a very astute 6-year-old. The strain was originally dubbed "swine flu", but the WHO hastily substituted "influenza A(H1N1)" after initial reports on “swine flu” resulted in a backlash against the pork industry, including the culling of all pigs in Egypt. (Cooking pork kills viruses, so the disease cannot be caught eating pork meat. I suppose that if an infected pig was processed in unhygienic conditions, and the meat was covered with pork respiratory secretions, and you stuffed the raw meat up your nose, there might be a chance of a problem. Presumably snorting raw infected pork is not a common pastime. Also, notably, although there are genetic indications that it is related to an endemic strain of swine influenza there is as yet no report of outbreak among livestock.) For more on the naming controversy, see http://blogs.sciencemag.org/scienceinsider/2009/05/swine-flu-names.html
Other footnotes and sources:
* Despite vigilant public heath campaigns to increase seasonal influenza vaccination rates among the elderly, studies in the U.S. and Italy has found that paradoxically there has been no decrease in deaths among those over age 65 as vaccination rates have gone up. A plausible hypothesis for this is that immune response to vaccines becomes less efficient as one grows older, so increasing vaccination among seniors reaches a point of diminishing returns. In light of this, public health officials are considering re-focusing vaccination strategy on younger members of the population who come in contact with the elderly, thereby protecting seniors by proxy. For more details, see http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=18959475
Avian influenza A(H5N1) is different strain novel swine flu, which is influenza A(H1N1). The avian influenza strain is being monitored as a potential pandemic strain. WHO statistics indicate that through 2009, there have been 423 laboratory-confirmed human cases of avian influenza A(H5N1) and 258 deaths worldwide, which is fairly low suggesting inefficient human-to-human transmission thus far, but the lethality rate is an alarming 61%. Recall that it’s 0.1% for normal seasonal influenza. http://www.who.int/csr/disease/avian_influenza/country/cases_table_2009_05_06/en/index.html
Source of statistics for Table 1: HIV/AIDS, Yale AIDS Watch (http://www.yale.edu/yaw/world.html); rabies, World Health Organization (http://www.who.int/mediacentre/factsheets/fs099/en/); ebola, World Health Organization (http://www.who.int/mediacentre/factsheets/fs103/en/); seasonal influenza, World Health Organization (http://www.who.int/mediacentre/factsheets/fs211/en/); 1918-1919 influenza pandemic, Tumpey TM and Belser JA (2009) Resurrected pandemic influenza viruses. Annual Reviews of Microbiology 63:79-98; Taubenburger JK and Morens DM http://www.cdc.gov/ncidod/eid/vol12no01/05-0979.htm.
Update, May 11, 2009: A research article on the initial epidemiological analysis of the swine influenza A(H1N1) strain confirms that the outbreak appears to be behaving in pandemic fashion, not seasonal fashion. Clinical severity seems on par with the 1957 pandemic, but not the 1918 pandemic. The epicenter of the outbreak has been narrowed to La Gloria, Veracruz, Mexico.
Image credit: Centers for Disease Control, Negative stain EM image of the swine influenza A/CA/4/09. http://www.cdc.gov/media/subtopic/library/diseases.htm


1 Comments:
Good article, Robyn.
Post a Comment
<< Home